OUR TREATMENTS
Dr. Deepak Vashistha brings years of expertise to the field of orthopedic surgery. He is known for his compassionate approach, thorough evaluation, and personalized treatment plans. Dr. Vashistha specializes in a wide range of orthopedic procedures, including joint replacements, sports injuries, spine surgery, and more.
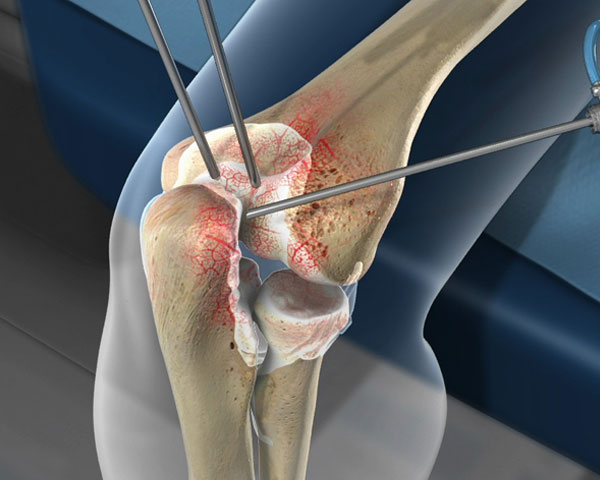
KNEE REPLACEMENT
Knee replacement surgery, a common orthopedic procedure, involves replacing damaged or worn-out knee joints with artificial implants. The surgery is typically recommended for individuals with severe arthritis, joint degeneration, or injuries causing significant pain and impaired mobility. During the procedure, the damaged surfaces of the knee joint are removed and replaced with prosthetic components. This surgery aims to alleviate pain, restore joint function, and improve overall quality of life. Patients undergo a thorough pre-operative evaluation to determine candidacy, and the surgery itself is performed under anesthesia. Recovery involves post-operative care, physical therapy, and gradual return to normal activities. Knee replacement has a high success rate, providing long-lasting relief for many individuals. While risks and complications exist, advancements in surgical techniques and prosthetic materials contribute to improved outcomes. Consultation with a qualified orthopedic surgeon helps determine the most suitable approach for individual cases.
Types of Knee Replacement
Total Knee Replacement
- Customized Implants: Tailored to individual anatomy, personalized implants enhance stability, comfort, and overall joint performance.
- Minimally Invasive Approaches: Utilizing minimally invasive methods when applicable, surgeons aim to reduce recovery time, minimize scarring, and promote faster healing.
- Pain Management Protocols: Comprehensive pain management strategies are integrated to ensure patient comfort during and after surgery, enhancing the overall recovery experience.
- Rapid Rehabilitation Programs: Structured rehabilitation plans and physical therapy facilitate early mobilization, fostering quicker recovery and improved joint functionality.
- Multidisciplinary Care Team: A collaborative approach involving orthopedic surgeons, physiotherapists, and other healthcare professionals ensures comprehensive pre-operative assessment and post-operative care.
- Cutting-edge Technology: Incorporation of state-of-the-art technologies, such as computer-assisted navigation, enhances surgical precision and improves implant alignment.
- Patient Education and Support: Informative pre-operative consultations and ongoing post-operative guidance empower patients, promoting active participation in their recovery journey.
- Proactive Infection Control Measures: Stringent infection prevention protocols are implemented to minimize the risk of post-operative infections and enhance patient safety.
- Long-term Follow-up Care: A commitment to long-term follow-up care ensures ongoing monitoring, addressing any potential issues, and promoting sustained joint health and function.These key features collectively contribute to the success and effectiveness of Total Knee Replacement surgery, providing patients with a renewed quality of life.
These key features collectively contribute to the success and effectiveness of Total Knee Replacement surgery, providing patients with a renewed quality of life.
Partial Knee Replacement
A partial knee replacement, or unicompartmental knee arthroplasty, is a surgical procedure replacing only a damaged knee compartment with an artificial implant. It’s suitable for localized arthritis. Benefits include a smaller incision, faster recovery, and a more natural feel. Physical therapy is crucial for rehabilitation. While not suitable for all cases, it offers relief for the right candidates, with longevity varying. Consultation with an orthopedic surgeon is essential for personalized advice.
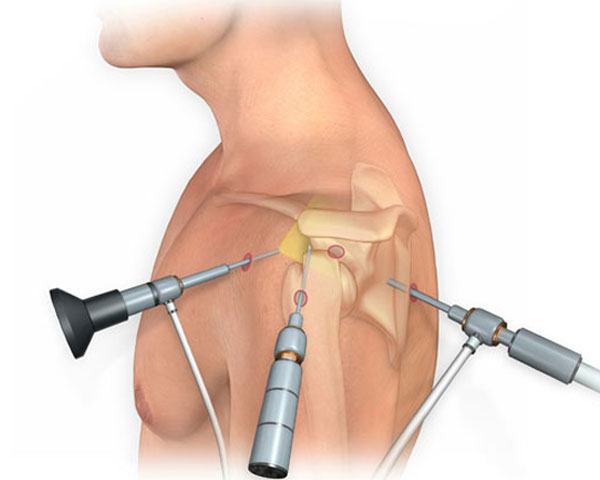
SHOULDER SURGERY
“Shoulder surgery” is a broad term that encompasses various surgical procedures aimed at addressing issues or injuries affecting the shoulder joint. The shoulder is a complex joint with a wide range of motion, and surgery may be recommended for different reasons. Here are some common types of shoulder surgeries:
- Rotator Cuff Repair: The rotator cuff is a group of muscles and tendons that stabilize the shoulder joint. Tears or injuries to the rotator cuff may require surgical repair, either through open surgery or arthroscopic techniques.
- Shoulder Arthroscopy: This minimally invasive procedure involves the use of a small camera (arthroscope) and specialized instruments to diagnose and treat various shoulder conditions, such as rotator cuff tears, labral tears, and inflammation.
- Labral Repair: The labrum is a cartilage ring that surrounds the shoulder socket. Tears or damage to the labrum may necessitate surgical repair, often done arthroscopically.
- Shoulder Replacement (Arthroplasty): In cases of severe arthritis or joint damage, shoulder replacement surgery may be considered. This involves replacing the damaged parts of the shoulder joint with artificial components.
- Shoulder Stabilization: Individuals with recurrent shoulder dislocations may undergo surgery to stabilize the shoulder joint, often through procedures like Bankart repair or Latarjet procedure.
- AC Joint Reconstruction: The acromioclavicular (AC) joint is where the collarbone meets the shoulder blade. Injuries or arthritis affecting this joint may require surgical reconstruction.
- Frozen Shoulder Release (Manipulation Under Anesthesia): For individuals with adhesive capsulitis or a frozen shoulder, a procedure called manipulation under anesthesia may be performed to break up adhesions and improve range of motion.
- Fracture Repair: Surgery may be necessary to repair fractures or breaks in the bones of the shoulder, such as the humerus or collarbone.
Recovery from shoulder surgery varies depending on the type and complexity of the procedure. Physical therapy is often a crucial part of the rehabilitation process to regain strength, mobility, and function in the shoulder.
Before undergoing any shoulder surgery, individuals should consult with an orthopedic surgeon who can assess the specific condition, discuss treatment options, and provide information about the risks and benefits associated with the chosen surgical approach.
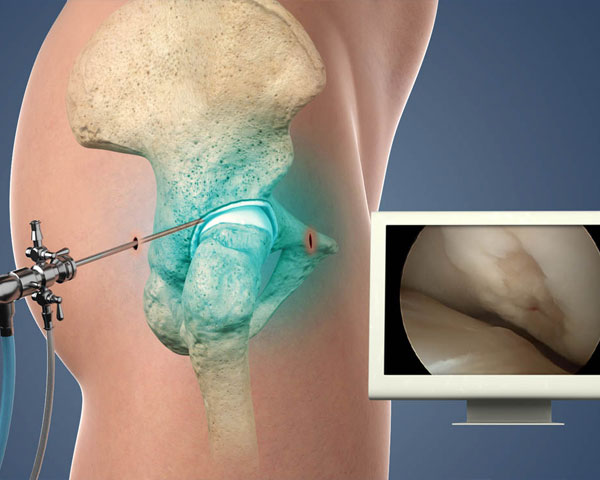
HIP TRANSPLANT
Hip replacement or hip arthroplasty, is a surgical procedure where a damaged or diseased hip joint is replaced with an artificial joint. This is often done to relieve pain and improve mobility in cases of severe hip conditions like osteoarthritis or fractures. The surgery involves replacing the damaged femoral head and acetabulum with artificial components, restoring joint function. While it’s an effective treatment, it’s a major procedure with associated risks and requires a period of rehabilitation and physical therapy for recovery.
Conditions of Hip replacement
Hip replacement is considered for conditions such as severe osteoarthritis, rheumatoid arthritis, post-traumatic arthritis (resulting from injury), avascular necrosis, hip fractures, congenital hip disorders, ankylosing spondylitis, and other degenerative joint diseases. When conservative treatments fail to alleviate symptoms and significantly impact daily life, hip replacement surgery may be recommended to relieve pain and improve mobility.
Why it’s done
Hip replacement is recommended for individuals experiencing severe hip joint conditions that significantly impact their quality of life. Common reasons for hip replacement include:
- Osteoarthritis: The degeneration of joint cartilage, leading to pain and reduced mobility.
- Rheumatoid Arthritis: An autoimmune disease causing inflammation and joint damage.
- Post-Traumatic Arthritis: Arthritis resulting from hip injury or fracture.
- Avascular Necrosis: Loss of blood supply to the hip joint, causing bone tissue death.
- Hip Fractures: Severe fractures of the hip joint may necessitate replacement.
- Congenital Hip Disorders: Birth defects or developmental issues affecting the hip joint.
- Ankylosing Spondylitis: Inflammatory arthritis affecting the spine and hip joints.
- Other Degenerative Joint Diseases: Conditions leading to hip joint degeneration and dysfunction.
When conservative treatments fail and symptoms severely impact daily activities, hip replacement surgery is considered to relieve pain, restore function, and improve overall quality of life.
Risk of Hip Replacement
While hip replacement surgery is generally considered safe and successful, like any surgical procedure, it does carry some risks and potential complications. It’s essential for individuals considering hip replacement to be aware of these risks, which may include:
- Infection: There is a risk of infection at the surgical site or in the artificial joint. Precautions, such as antibiotics, are taken to minimize this risk.
- Blood Clots: Deep vein thrombosis (DVT) and pulmonary embolism (PE) are potential complications, and measures such as blood thinners and early mobilization are used to prevent them.
- Dislocation: The artificial joint may dislocate, especially in the first few months after surgery. Precautions and specific movements are advised to reduce this risk.
- Implant Wear: Over time, the artificial joint may experience wear and tear, potentially leading to the release of tiny particles. In some cases, this can cause inflammation and damage to the surrounding tissues.
- Nerve and Blood Vessel Damage: Injury to nearby nerves or blood vessels during surgery is a rare but serious risk.
- Leg Length Inequality: There is a possibility of a slight difference in leg length after surgery.
- Allergic Reactions: Some individuals may have allergic reactions to materials used in the artificial joint.
- Pain: Persistent or new-onset pain is a potential complication, although it’s usually temporary.
- Limited Range of Motion: Some individuals may experience a reduced range of motion in the replaced hip.
- Anesthesia Risks: Complications related to anesthesia, such as respiratory or cardiovascular issues, can occur.
Symptoms of Hip Replacement
Hip joint problems can manifest with various symptoms, and the severity and specific symptoms can vary depending on the underlying cause. Common symptoms of hip joint problems include:
Pain:
- Persistent or intermittent pain in the hip joint, groin, thigh, or buttocks.
- Pain may worsen with activity or movement, and it can interfere with daily tasks.
Stiffness:
- Reduced range of motion in the hip joint.
- Difficulty in performing activities that involve hip movement, such as bending or tying shoelaces.
Swelling:
- Inflammation and swelling around the hip joint.
Clicking or Popping:
- Audible sounds or sensations (clicking, popping, or grinding) when moving the hip joint.
Limping:
- Changes in gait or the development of a noticeable limp.
Instability:
- Feeling of instability or a sensation that the hip may give way.
Limited Mobility:
- Difficulty in performing activities that require flexibility or mobility in the hip joint.
Pain at Rest:
- Discomfort or pain even when at rest, especially during periods of inactivity or while sleeping.
Radiating Pain:
- Pain that may radiate from the hip to the buttocks, thigh, or knee.
Difficulty in Weight-Bearing:
- Difficulty putting weight on the affected hip.
Hip Replacement Procedure
The hip replacement procedure involves several key steps:
Preparation:
- The patient is positioned on the operating table, and anesthesia (either general or regional) is administered to ensure the patient is comfortable and pain-free during the surgery.
Incision:
- A surgical incision is made over the hip joint, providing access to the damaged joint.
Removal of Damaged Tissue:
- The damaged femoral head is removed from the thigh bone (femur).
- The damaged cartilage and bone in the acetabulum (hip socket) are also removed.
Placement of the Prosthesis:
- An artificial femoral component, consisting of a metal stem with a ball at the end, is inserted into the femur.
- A prosthetic socket, usually made of metal, plastic, or ceramic, is implanted into the acetabulum.
Attachment and Testing:
- The artificial ball and socket are connected, creating the new hip joint.
- The surgeon checks the range of motion and stability of the new joint.
Closure:
- The incision is closed with stitches or staples.
Recovery and Rehabilitation:
- The patient is monitored in the recovery room before being transferred to a regular hospital room.
- Physical therapy and rehabilitation begin shortly after surgery to promote healing, regain strength, and ensure proper function of the new hip joint.
It’s important to note that recovery times can vary, and patients are typically advised to avoid certain activities and follow rehabilitation guidelines provided by their healthcare team to optimize the outcome of the hip replacement surgery.

SPORTS INJURIES
A sports injury refers to damage or harm to the body that occurs during sports or exercise activities. These injuries can affect bones, muscles, ligaments, tendons, and other structures, and they may range from mild to severe. Sports injuries can result from various factors, including accidents, overuse, improper training techniques, or inadequate warm-up.
Types
Common types of sports injuries include:
- Sprains and Strains: Sprains involve the stretching or tearing of ligaments (connecting bone to bone), while strains involve damage to muscles or tendons (connecting muscle to bone). These injuries often occur due to sudden movements or overexertion.
- Fractures: Broken bones can result from impact or excessive force during sports activities. Stress fractures, which are tiny cracks in the bone, can also occur with repeated stress.
- Dislocations: A dislocation happens when the bones in a joint are forced out of their normal positions. This can occur in joints like the shoulder or knee and is often a result of a traumatic incident.
- Tendon Injuries: Tendons connect muscles to bones, and injuries such as tendonitis (inflammation) or tendon ruptures can occur, often due to overuse or repetitive motions.
- Concussions: Head injuries, including concussions, can happen in contact sports. Concussions result from a blow to the head, causing temporary impairment of brain function.
- Overuse Injuries: Repetitive motions or excessive training without adequate rest can lead to overuse injuries such as stress fractures, tendinitis, or bursitis.
- Contusions (Bruises): Impact or blunt force can cause bruises, which are the result of broken blood vessels under the skin.
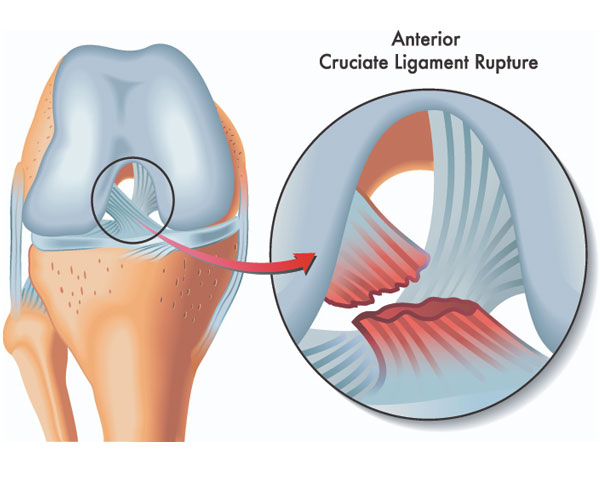
- Ligament Injuries: Injuries to ligaments, such as the anterior cruciate ligament (ACL) in the knee, are common, often occurring during sudden stops or changes in direction.
Preventing sports injuries involves proper training techniques, warm-up and cool-down routines, the use of protective gear, and maintaining overall fitness. Treatment for sports injuries varies depending on the type and severity but may include rest, ice, compression, elevation (R.I.C.E.), physical therapy, and in some cases, surgical intervention.
Prompt and appropriate medical attention is crucial for managing sports injuries to minimize long-term consequences and facilitate a speedy recovery. Athletes and individuals engaging in physical activities should prioritize safety, listen to their bodies, and seek professional guidance for injury prevention and rehabilitation.
Sports Injury Treatments
The treatment of sports injuries can vary depending on the type and severity of the injury. Here are some common treatments for sports injuries:
Rest: Rest is often the first line of treatment for many sports injuries. It allows the body to begin the healing process by minimizing stress on the injured area.
Ice: Applying ice to the injured area helps reduce swelling and numbs the pain. This is typically done in the first 48 hours following an injury.
Compression: Compression with bandages or compression sleeves helps control swelling and provides support to the injured area.
Elevation: Elevating the injured limb or body part helps reduce swelling by allowing fluids to drain away from the injured area.
Physical Therapy: Many sports injuries benefit from rehabilitation through physical therapy. Therapists design exercise programs to improve strength, flexibility, and range of motion.
Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, may be recommended to manage pain and inflammation. In some cases, prescription medications may be necessary.
Bracing and Supports: Splints, braces, or supports may be used to stabilize and protect the injured area during the healing process.
Casting or Immobilization: For more severe injuries or fractures, casting or immobilization may be necessary to allow proper healing.
Injections: In certain cases, corticosteroid injections may be administered to reduce inflammation and alleviate pain.
Surgery: Some sports injuries, particularly severe ligament tears or fractures, may require surgical intervention. Surgery is often considered when conservative measures fail to provide relief or when the injury is deemed severe.
Regenerative Medicine: Emerging treatments, such as platelet-rich plasma (PRP) therapy and stem cell therapy, aim to promote tissue healing and regeneration. These treatments are still under investigation for their effectiveness in sports injury management.
It’s important for individuals with sports injuries to consult with healthcare professionals, such as orthopedic specialists or sports medicine doctors, for a proper diagnosis and treatment plan tailored to their specific condition. Early and appropriate intervention can contribute to a faster and more effective recovery, reducing the risk of long-term complications.
SPORTS INJURIES
Ligament injuries occur when there is damage to the tough bands of connective tissue that connect bones to other bones, providing stability to joints. Ligaments are crucial for joint function, and injuries to these structures are common, especially in activities that involve sudden stops, changes in direction, or impacts. Some common types of ligament injuries include:
Sprains: Ligament sprains are the most common type of ligament injury. They occur when a ligament is stretched or torn. The severity of a sprain is often graded on a scale from mild (Grade I) to severe (Grade III).
- Grade I Sprain: Mild stretching or microscopic tearing of the ligament. Minimal loss of function.
- Grade II Sprain: Partial tearing of the ligament. Moderate loss of function and stability.
- Grade III Sprain: Complete tearing of the ligament. Significant loss of function and stability.
Torn Ligaments: Ligaments can be partially or completely torn due to trauma or excessive force. Common examples include torn anterior cruciate ligament (ACL) in the knee or torn rotator cuff ligaments in the shoulder.
Overuse Injuries: Repetitive stress on ligaments, often from activities like running or jumping, can lead to overuse injuries. These may manifest as chronic pain, inflammation, or degeneration of the ligament.
Ligamentous Instability: In some cases, ligament injuries can result in joint instability. This can make the affected joint feel loose or wobbly and may lead to a higher risk of future injuries.
Common causes of ligament injuries include sports-related activities, falls, motor vehicle accidents, and sudden twists or impacts. The symptoms of a ligament injury may include pain, swelling, bruising, and difficulty moving the affected joint.
Treatment for ligament injuries depends on the severity and type of injury but may include:
- Rest, Ice, Compression, Elevation (R.I.C.E.): This approach is often used for mild to moderate ligament injuries to reduce swelling and promote healing.
- Physical Therapy: Exercises to strengthen the muscles around the injured ligament and improve joint stability.
- Bracing or Splinting: Provides support to the injured joint during the healing process.
- Medications: Pain relievers and anti-inflammatory drugs may be recommended.
- Surgery: In some cases, especially for severe ligament tears, surgical intervention may be necessary to repair or reconstruct the ligament.
Prompt and appropriate medical attention is crucial for the proper diagnosis and management of ligament injuries. Severe or untreated ligament injuries can lead to long-term joint problems and increased risk of re-injury.
Why its done
Ligament repair or reconstruction is done for several reasons, primarily to address injuries or conditions affecting the ligaments. The most common motivations for undergoing ligament surgery include:
Ligament Tears or Ruptures: Ligaments can be torn or ruptured due to trauma, sports injuries, or accidents. In cases where the tear is severe or if there is a complete rupture, surgery may be necessary to repair or reconstruct the ligament.
Joint Instability: Ligaments play a crucial role in stabilizing joints. If a ligament is damaged or weakened, it can lead to joint instability. Ligament repair or reconstruction is performed to restore stability to the affected joint and prevent further damage.
Chronic Pain: Some individuals may experience chronic pain due to ligament injuries or conditions. Surgery may be recommended to address the underlying issue and alleviate persistent pain.
Degenerative Conditions: Over time, ligaments can undergo wear and tear, leading to degeneration. Conditions like osteoarthritis can affect the ligaments, and in some cases, surgery may be considered to manage symptoms and improve joint function.
Sports-Related Injuries: Athletes, particularly those involved in sports with high-impact or rapid direction changes, are prone to ligament injuries. Surgery may be recommended to restore optimal function and allow athletes to return to their sport.
Failed Conservative Treatment: In cases where conservative treatments such as rest, physical therapy, and medications fail to provide relief or restore function, surgery may be considered as the next step.
Preventative Measures: In some cases, individuals with a history of repeated ligament injuries or those at high risk of ligament injuries due to their anatomy or activity level may undergo preventive ligament surgery. This is especially common in the case of the anterior cruciate ligament (ACL) in the knee.
Common examples of ligament surgeries include ACL reconstruction in the knee, repair of torn ligaments in the ankle, and procedures to address ligament injuries in the shoulder or elbow.
The decision to undergo ligament surgery is typically based on a thorough evaluation by a healthcare professional, including considerations of the severity of the injury, the individual’s overall health, and their goals for recovery. It’s important for individuals to discuss their specific case with a qualified orthopedic surgeon or sports medicine specialist to determine the most appropriate course of action.
Risk of Ligament Injuries
Ligament injuries can result from a variety of factors, and certain activities or conditions may increase the risk of sustaining such injuries. Some common risk factors for ligament injuries include:
Sports Participation: Athletes, especially those involved in sports that require sudden stops, changes in direction, or jumping, are at a higher risk of ligament injuries. This includes sports like soccer, basketball, football, and skiing.
Previous Injuries: Individuals who have previously experienced ligament injuries are at a higher risk of re-injury. Proper rehabilitation and strengthening exercises are crucial to reduce this risk.
Improper Training Techniques: Poor training methods, including inadequate warm-up, overtraining, or incorrect techniques, can increase the risk of ligament injuries.
Muscle Imbalances: Weakness or imbalances in the muscles surrounding a joint can affect its stability, putting additional stress on ligaments and increasing the risk of injury.
Joint Laxity: Some individuals naturally have looser joints, a condition known as joint laxity or hypermobility. This increased flexibility can contribute to a higher risk of ligament injuries.
Age and Gender: Ligament injuries are more common in certain age groups, with adolescents and young adults being particularly susceptible. Additionally, research suggests that females may have a higher risk of certain ligament injuries, such as anterior cruciate ligament (ACL) tears, compared to males.
Environmental Factors: Uneven playing surfaces, inadequate footwear, or environmental conditions can contribute to an increased risk of ligament injuries.
Poor Nutrition and Hydration: Inadequate nutrition and dehydration can impact the strength and flexibility of ligaments, making them more susceptible to injury.
Trauma and Accidents: Falls, collisions, and accidents can result in sudden and forceful movements that may cause ligament injuries.
Occupational Factors: Certain occupations or activities that involve repetitive stress or strain on specific joints may increase the risk of ligament injuries over time.
Ligament Surgery
Ligament surgery is a medical procedure performed to address injuries or conditions affecting the ligaments, which are tough bands of connective tissue that connect bones to other bones, providing stability to joints. Ligament surgery may involve repair or reconstruction, depending on the nature and severity of the ligament injury. Here are some key aspects of ligament surgery:
Types of Ligament Surgery:
- Ligament Repair: In cases where the ligament is partially torn, a surgeon may opt to repair the ligament by suturing the torn ends together. This is often considered for certain types of tears and if the ligament has the potential to heal on its own.
- Ligament Reconstruction: When a ligament is severely torn or completely ruptured, reconstruction may be necessary. This involves replacing the damaged ligament with a graft, which can be obtained from the patient’s own tissue (autograft) or from a donor (allograft).
Common Ligament Surgeries:
- Anterior Cruciate Ligament (ACL) Reconstruction: A common procedure, especially among athletes, to address a torn ACL in the knee.
- Posterior Cruciate Ligament (PCL) Reconstruction: Similar to ACL reconstruction, this surgery focuses on the PCL in the knee.
- Lateral Collateral Ligament (LCL) or Medial Collateral Ligament (MCL) Reconstruction: These procedures are performed to address injuries to the collateral ligaments of the knee.
- Rotator Cuff Repair: While not a ligament, the rotator cuff in the shoulder consists of tendons that are commonly repaired surgically to address tears.
Surgical Techniques:
- Arthroscopic Surgery: Many ligament surgeries are performed arthroscopically, using small incisions and a tiny camera (arthroscope) to guide the surgeon. This minimally invasive approach often results in quicker recovery times.
- Open Surgery: In some cases, particularly for more complex injuries, traditional open surgery may be necessary.
Rehabilitation and Recovery:
- Following ligament surgery, rehabilitation is a crucial aspect of the recovery process. Physical therapy helps restore strength, flexibility, and range of motion.
- The recovery timeline varies depending on the type of surgery, the specific ligament involved, and individual factors. It may take several months for full recovery.
Risks and Complications:
- As with any surgery, there are potential risks and complications, including infection, bleeding, and adverse reactions to anesthesia.
- Graft failure, persistent pain, or limited range of motion are potential complications that may require further intervention.
Postoperative Care:
- Patients are typically given postoperative care instructions, including pain management, wound care, and guidelines for physical therapy exercises.
- Follow-up appointments with the surgeon are scheduled to monitor progress and address any concerns.
Ligament surgery is often considered when conservative treatments, such as rest and physical therapy, have not provided adequate relief, and the goal is to restore stability and function to the affected joint. The decision to undergo surgery is made based on a thorough evaluation by a healthcare professional, taking into account the nature of the injury, the individual’s health, and their activity level.

